“I love everything in the world … except for ticks.” – The Dalai Lama
New England has the highest incidence of Lyme disease in the world, with Martha’s Vineyard and Westchester, NY leading the way. This summer we will have another difficult season with Lyme and other tick-borne diseases. The winter was not cold enough to reduce populations of ticks, or starve the white-footed mice, the main, but not exclusive, host of the Lyme tick in the Northeast.
New England has the highest incidence of Lyme disease in the world, with Martha’s Vineyard and Westchester, NY leading the way. Share on X
Lyme Disease is an Epidemic
Lyme disease is the most common tick-borne disease in North America and Europe, and one of the fastest-growing infectious diseases in the United States. (CDC MMWR). The CDC estimates 400,000 cases of Lyme disease this year. Ten years ago, the estimate was 30,000. The 400,000 number is based on surveys of clinical labs and medical claims. Since 1/3 of patients never have a rash or recall a tick bite, and others don’t seek care for “summer flu,” 400,000 is a spectacular underestimate. I would guess the real number is >1,000,000 cases. Epidemic growth is also worldwide – the incidence of Lyme disease in England increased 42% from 2011 to 2015.
A Quick Guide to the Tick Lifecycle
As forests have been turned into suburban neighborhoods, nesting areas for white-footed mice were created, while habitats for the mouse’s predators — foxes, coyotes, and owls — were destroyed. The population of mice, which breed every three weeks, has risen into the billions. Their nests serve as incubators for developing Lyme ticks.
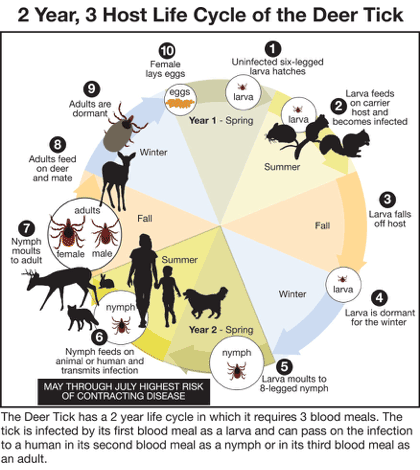
Tick larvae are born uninfected. They feed on blood from the white-footed mice (and chipmunks and short-tailed shrews) and acquire Borrelia bacteria, the cause of Lyme disease. They can feed on birds or other rodents, which do not carry the Lyme bacteria, and remain uninfected. The larvae grow into nymphs, which seek a second blood meal from a larger animal, such as foxes, livestock, dogs, or humans. With this bite, the tick injects borrelia. For its last meal, the tick, now an adult, latches onto a very large animal, predominantly, but not exclusively, the white-tailed deer for nourishment to mature and produce eggs. Legislated protections have enlarged deer herds, increasing the reservoir for adult ticks. Once mature, each female produces 3,000 eggs, and dies. These eggs will hatch into larvae, which will find their way to white-tailed mice, who will bring them back to their nests. Warmer winters, more nesting areas, fewer mouse predators, and increased deer populations is a recipe for creating huge pools of ticks.
Problems Diagnosing Lyme Disease
The vast majority of Lyme infections are spontaneously cleared by the body. However, Borrelia bacteria are spirochetes (spiral-shaped), which can avoid our bodies’ primary immune defenses and conceal themselves in lymph nodes and neurologic tissue, and so lie dormant or cause chronic infections. Tests for infections are immunologic, and the significant rate of false negative tests leads to people being incorrectly told they don’t have Lyme or being undertreated. This led to the rise of private specialty labs, some of whom were fined or closed by state and federal authorities for reporting excess false positive results. There is a genetic test under evaluation that appears to be phenomenally accurate, much like criminal DNA tests.
The significant rate of false negative tests leads to people being incorrectly told they don’t have Lyme. Share on X
Medical Costs
Among patients who sought treatment, medical costs in the US in 2015 were about 3.1 billion dollars. In addition, non-medical costs, such as lost work, disability, pain and suffering, and lost outdoor recreation opportunities due to fear of Lyme, were estimated at 5 billion dollars by the Yale Forestry School. True costs are higher still because the Lyme tick can also transmit anaplasmosis, babesiosis, ehrlichiosis, and Powassen Fever. While significantly less frequent than Lyme, these diseases are more severe, more expensive to treat, more frequently disabling, and occasionally lethal.
The cost of Post-Treatment Lyme Disease Syndrome (once called Chronic Lyme Disease) is not in this estimate. It is a controversial diagnosis, without reliable criteria, and with low concordance between practitioners. While it certainly exists, one needs a specialist who is more doctor than politician. The correct treatment for Post-Treatment Lyme Disease Syndrome (PTLDS) is problematic. I have already explained the problems with existing laboratory testing. Patients can have a coinfection with anaplasmosis, babesiosis, ehrlichiosis, or Powassen Fever, and present with an ambiguous clinical picture. Lastly, both the Borrelia bacteria, as well as some of the coinfectors have variable responses to antibiotics, so some people remain infected after treatment. These cases are rare; the benefits of IV antibiotics beyond 30 days rarely justifies the risks.
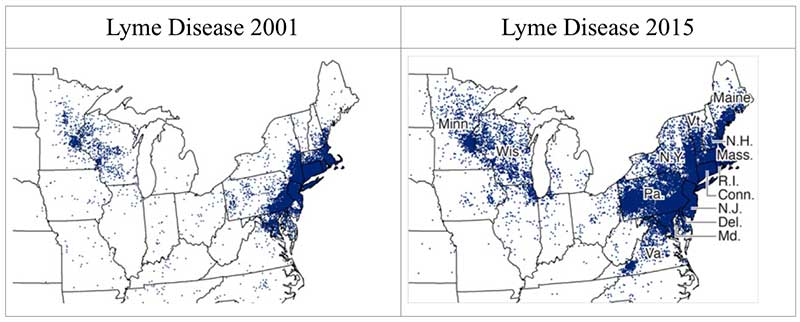
The CDC’s failure to appreciate the extent of the Lyme problem lent credibility to internet trolls. However, guidelines for Lyme treatment now include IV antibiotics in appropriate cases. My point, later in this essay, is to avoid Lyme treatment issues by killing the ticks before they can infect you. Below is a map of Lyme disease in the US: however, if we include all the other tick-borne diseases, the map would be covered from end to end.

Note: This map demonstrates an approximate distribution of predicted Lyme disease risk in the United States. The true relative risk in any given county compared with other counties might differ from that shown here and might change from year to year. Information on risk distribution within states and counties is best obtained from state and local public health authorities.
The Best Tick Bite is the One that Never Happens.
Below are the standard measures to avoid tick bites, or remove one before it can transmit the Borrelia bacteria. Injection of Borrelia from the tick’s gut takes place at the end of 24-48 hours of feeding, after which the tick releases its grip on the skin and falls off. However, the other four infective agents — anaplasmosis, ehrlichiosis, babesiosis, and Powassen fever — are carried in the tick’s salivary glands and are injected when the tick bites.
The CDC emphasizes attire and DEET, which will decrease tick bites.
- Wear long pants, stick them into your socks. Wear long-sleeved shirts.
- Stay on trails, do not walk near tall grass, and avoid touching branches.
- Shower or bathe as soon as possible after being outdoors.
- Conduct a full-body tick check.
- Check your pets, backpacks, etc.
 This advice fails because ticks are nearly invisible. Here is a picture of a deer tick. It is the size of a poppy seed. It can climb onto your shoe, up your socks, then under your clothing, up to armpits, back, or scalp. Or get on your clothing if you walk through tall grass. Its bite is painless. Its specialty is stealth. 30% of patients with Lyme disease do not report ever being bitten. Mr. Tick is hard to spot.
This advice fails because ticks are nearly invisible. Here is a picture of a deer tick. It is the size of a poppy seed. It can climb onto your shoe, up your socks, then under your clothing, up to armpits, back, or scalp. Or get on your clothing if you walk through tall grass. Its bite is painless. Its specialty is stealth. 30% of patients with Lyme disease do not report ever being bitten. Mr. Tick is hard to spot.
After how to dress, the CDC recommends 20% DEET, applied directly to skin, as a repellent (on children, avoid the face and hands). Deer ticks will not attach to skin covered in DEET. But they will walk around the DEET area till they find an untreated area. DEET must be reapplied more than once a day to be effective, and people forget to reapply it. One can use picardin, a black pepper derivative, if one wishes to avoid DEET, but picardin has similar limitations.
Deer ticks are nearly invisible. 30% of patients with Lyme disease do not report ever being bitten. Share on X
Permethrin — Kill the Damn Tick before it Bites!
Which brings us to Permethrin, the least used and most effective agent. Permethrin was developed to make natural pyrethrum from chrysanthemums more stable in sunlight. Permethrin has many uses — head lice shampoos; flea, tick and mosquito control on dogs; mosquito control for outdoor clothing and camping gear; and landscape pest control. (livingwithbugs.com) I know organic farmers who wear permethrin-treated clothing out in their fields.
 It is sprayed on clothing, not skin, because it is sticky, uncomfortable, and can cause rashes. Directions are simple; spray for 30 seconds on each area of fabric to be treated and let dry for 2 hours or overnight if humidity is very high. Below are my favorite garden jeans. Can you tell which leg was treated? (It is the right leg — and right shoe)
It is sprayed on clothing, not skin, because it is sticky, uncomfortable, and can cause rashes. Directions are simple; spray for 30 seconds on each area of fabric to be treated and let dry for 2 hours or overnight if humidity is very high. Below are my favorite garden jeans. Can you tell which leg was treated? (It is the right leg — and right shoe)
Once applied, it remains effective for several months; and if the clothes are not frequently washed, it will last a year. Permethrin-treated clothing kills ticks and mosquitoes on contact — i.e. before they bite. Killing, rather than repelling, ticks reduces the risk of all tick and all mosquito-borne diseases. On the East coast, the tick diseases include Lyme, babesiosis, anaplasmosis, ehrlichosis, and Powassen. The local mosquito diseases include Zika, West Nile Virus, Equine Encephalitis, and dog heartworm. Four of these can be fatal. Why risk acquiring any of these?
Some ready-to-wear options:
Solstice Apparel Women’s Insect Repellent Convertible Pants
ExOfficio Women’s Bugsaway Lumen Hoodie
Solstice Apparel Men’s Insect Repellent Convertible Pants
Insect Shield Mesh Tank Top for Dogs
Is It Safe?
Permethrin is the active ingredient in lice/scabies medicines like Nix and Elimite, which are approved for treatment of children as young as 3 months, as well as for pregnant or nursing mothers. It is FDA Category B in pregnancy — it’s highest safety rating. It has near zero absorption from treated clothing; wearing permethrin-treated clothing for 28 consecutive days did not result in significant blood or urine levels. Organizations from The National Academy of Sciences to the US Army endorse it. In comparison with the other toxins people are exposed to every day (gasoline fumes, air pollution, etc.) permethrin is benign. The EPA “RED” sheet states permethrin “does not represent increased risk.”
It is toxic to fish and cats, but not dogs, horses, other animals, or people. There are some internet sites that insist its safety isn’t proven (Beyondpesticides.org). As a physician certified in Occupational and Emergency medicine, I know quite a bit about toxic substances. Your household cleansers are more dangerous than permethrin.
Nothing is risk-free, so the appropriate question is risk/risk — risk of permethrin versus risk of infection. Patients’ individual preferences are a crucial part of these decisions — example; for a senior citizen, cost may be the determining factor, while for the parent of a small child, safety may be key. But if one looks at the extent of tick and mosquito disease, in numbers, in cost, and in suffering, and one lives in the Northeast US, in my opinion, the equation favors permethrin.
Is It Effective?
Permethrin reduces the incidence of tick bites by over 80% (UNC Study of Forest Rangers in American Journal of Preventive Medicine, 2014). Both the treatment group and controls were experienced outdoor workers who used conventional repellents like DEET and proper clothing. The permethrin-treated clothing group had a remarkable reduction in ticks on daily inspections, and a marginally lower rate of new infections. Peak incidence of new cases of Lyme occurs in 5- to 15-year olds, or people over 55. The average forest ranger is skilled at avoiding ticks; I would project significantly better percentage improvement for children and adults who do not have experience or special training.
My recommendation is to give your outdoor shoes, socks, leggings, and pants a permethrin treatment when you buy them and annually thereafter. Also treat outdoor lounge chairs, furniture, and carpets. Let them dry overnight. That one treatment is good for up to two years (depending on how often it rains on the furniture or how often you wash the clothes) or 10 washings. Professionally treated clothing maintains insecticide potency for 70 wash cycles. Put a note on your Google calendar or smartphone to treat again annually. Organic farmers get their permethrin from https://sawyer.com/products/permethrin-premium-insect-repellent/ or Amazon: https://www.amazon.com/dp/B001ANQVYU/
This military video has instructions for home application. Permethrin treatment is standard for US and British military troops operating in applicable climates. One can order permethrin-treated clothing from Recreational Equipment Inc., Cabela’s, L.L. Bean, or Amazon. Consumer Reports has a study showing the clothing works and finds no safety issues with permethrin.
Strategy: Part Four — Always Look
However good permethrin-treated clothing might be, there is no substitute for a tick inspection after being outdoors in grassy areas. A friend recently had to get antibiotic treatment when he discovered an engorged tick under his watchband. Your pets can bring tics in on their fur, and they’re also prone to Lyme disease. Why every garden club, school, recreational program, or home landscaper does not promote permethrin use is a great public health question. To stop the disease, one must spot the tick (that one never felt or saw) and remove it. The tick check is the last line of defense.
Strategy: Part Five — Kill the Ticks Where They Nest
Eastern ticks breed primarily in the dens of white-footed mice. To kill the ticks before human exposure, one can target mice nests. Get some six-inch lengths of 2″ PVC pipe (or toilet paper rolls). Thoroughly spray big, fluffy cotton balls with permethrin, and let dry overnight. Wearing gloves (they will be sticky), stuff 4-6 cotton balls in each pipe, and place them at the base of leaf piles and stone walls. The mice will take the cotton balls to use as bedding in their nests. This can reduce tick populations by 90%. Reload/replace the pipes at least every three months, or when emptied.
Here is a link for commercially produced tick tubes. https://amzn.to/2IOdRVn
Ticks also reside on deer (that is how they got their name), so limiting deer populations can limit the number of ticks. This was successful on Monhegan Island in Maine. However, what works in a highly-confined space, like an island, does not work as well in open country. Deer are highly mobile; each one carries enough ticks to reconstitute an entire tick ecosystem. So culling deer herds has limited benefit.
Spraying yards with insecticide can tick populations, but the effect is brief. Mice build nests where sprayers can’t reach, and ticks can use many different species, like birds and squirrels, to move from place to place. Ticks reappear after the permethrin sprayed outdoors is washed away by rain or evaporates. Each surviving female tick can lay 3,000 eggs, so they can repopulate. While spraying for agricultural use under EPA guidelines is appropriate, I do not recommend spraying your yard. It is unlikely to penetrate the mouse nests and will result in increased groundwater presence, placing aquatic organisms at risk, as well as being toxic to honeybees, which are already threatened.
There is one missing item: a vaccine. There is an effective vaccine (Lymerix), which was withdrawn from the market at the peak of the anti-vaccine frenzy, amid threats of lawsuits for adverse reactions, which never materialized. You can get a vaccine for your dog in the US, just not one for you. You can get a vaccine for slightly different Borrelia bacteria in Europe. But there isn’t a vaccine in the US.
How Much Can We Save?
Here is where Science meets Politics. Each of the six states with the highest incidence of Lyme disease is facing cuts in their public health departments. These agencies must monitor infectious diseases, rape crisis programs, children with special needs, AIDS treatment, needle exchange programs, and multiple other priorities; not to mention the explosive opioid epidemic. With funding uncertain – possibly a public/private enterprise might be possible. Let’s look at a hypothetical test case.
Connecticut has about 30,000 new cases of Lyme disease per year. There an additional 10,000 cases for patients who never had a rash. An education program to precede distribution of permethrin would cost 2 million dollars and permethrin about 10 million dollars. If permethrin prevents 25% of cases, that is 10,000 cases of Lyme. However, based on the North Carolina study, the number would be closer to 20,000. The CDC estimates $3,000/treatment per case; medical savings would be $60,000,000. That is $5 saved for each $1 spent. However, reductions in other tick and mosquito-borne diseases will save additional dollars, and some lives. 50,000 medical office visits become available for other illnesses. Add the number days of disability, missed school, and other economic losses and the savings are over 100 million dollars. I will defer to economists for a final tally. For those who say a Lyme prevention program won’t move the needle on health care costs, recall former Senator Everett Dirksen, “A billion here, a billion there, and pretty soon you’re talking about real money.”
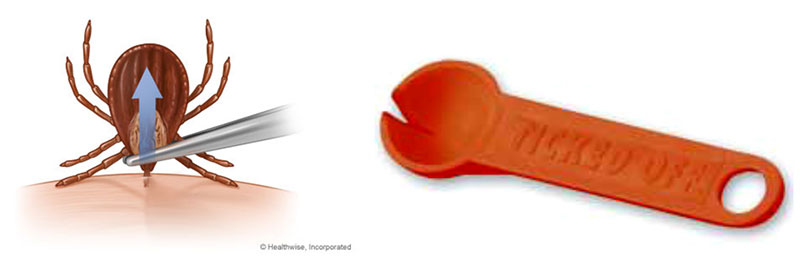
No essay on Lyme disease would be complete without instructions on removing a tick. Clean the area with alcohol. Crushing ticks is NOT advised — you risk injecting yourself with bacteria in the process. There are better removal tools. A fine tweezer can be used, or a tick spoon. Clean and scrub the area with soap and water when you are done, just like you would any other splinter. No burnt match heads, gasoline, Vaseline, etc., please!
You can buy a “Ticked Off” remover here: https://amzn.to/2IJTBZd
References
Testing Summary: Clinical Infectious Disease. Hinckley, A., Published online May 30, 2014.
“Health care costs, utilization and patterns of care following Lyme disease” Adrion, M;
John A, MD; Klaus Lemke, PhD; and Weiner, J, D.Ph., John’s Hopkins Bloomberg School of Public Health
Consumer Reports, May 26, 2016
The article “Long-lasting permethrin-impregnated uniforms: A randomized-controlled trial for tick bite prevention,” was published online April 16 in the American Journal of Preventive Medicine.
Incident Tick-Borne Infections in a Cohort of North Carolina Outdoor Workers. Vector Borne Zoonotic Dis. 2016 May;16(5):302-8. doi: 10.1089/vbz.2015.1887. Epub 2016 Mar 23.
The Allocation of Time and Risk of Lyme: A Case of Ecosystem Service Income and Substitution Effects Kevin Berry
Effectiveness of Residential Acaricides to Prevent Lyme and Other Tick-borne Diseases in Humans Alison F. Hinckley J Infect Dis (2016) 214 (2): 182-188
More reference available on request.
__________________
Reprint this story as you wish.
Some of the protective products mentioned in this article are listed below:

